Medicaid Unwinding Update
Earlier this summer, Legal Council reported on Medicaid Unwinding, a process in which the Illinois Department of Human Services (DHS) is reverting back to its pre-pandemic annual Medicaid redetermination process. During the Public Health Emergency (PHE), federal COVID-19 relief laws allowed states to pause termination and provide continuous coverage for Medicaid recipients. The process for Medicaid renewal requires Medicaid customers to submit their renewal forms for eligibility verification unless their eligibility can be renewed through electronic verification by the state.
It is important to remember that Medicaid enrollees will have different renewal deadlines throughout the next year.
How do Medicaid Customers Find their Renewal Date?
Online: abe.illinois.gov – Check your due date in your “Benefits Details” tab
- NOTE: The renewal form will be available one month before the renewal is due, and, if it is time to renew, customers will see a “Renew my Benefits” button on their “Case Summary” page.
Phone: 1-855-828-4995, this option is available 24 hours a day (English & Spanish) if the customer inputs their Recipient Identification Number (RIN) on their HFS-issued medical card.
- NOTE: Customers who are non-English or Spanish speakers can call 1-800-843-6154 to access a live interpreter to assist with translation
- If a redetermination done over the phone requires further verification documents, DHS will mail a checklist with a due date by which a customer should submit proof of eligibility.
30-Day Grace Period Update
In an effort to minimize the loss of coverage for customers who are still eligible during this redetermination process, the Centers for Medicare & Medicaid Services (CMS) approved a 30-day grace period. This flexibility delays case cancellations by approximately 30 days for customers who miss their redetermination deadline. This will remain in place until the end of the unwinding period set to end in May 2024.
The timeline for this process is outlined (below), with renewals sent for each month and the corresponding due dates, potential loss of coverage dates for ineligibility, and the grace period indicated.
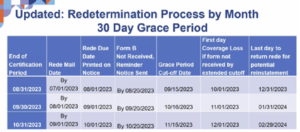
Source: Illinois Healthcare and Family Services
Legal Council commends the state’s goal of improving the accuracy and flexibility with this grace period for this redetermination process, as it will significantly reduce the risk of coverage loss for eligible customers. We will continue to monitor the Medicaid Unwinding process to avoid gaps in medical coverage for our communities to the greatest extent possible.