Navigating Medicaid Unwinding: Successes and Advocacy in Illinois
In recent years, you may have seen posts from Legal Council about the Public Health Emergency (PHE) and Medicaid Unwinding. During the PHE, federal COVID-19 relief changes allowed states to pause Medicaid terminations and redeterminations, allowing continuous enrollment. States are now going through Unwinding—ending these continuous enrollment provisions and returning to pre-pandemic annual Medicaid redeterminations. This redetermination process requires the state to verify eligibility electronically, and when that is not possible, customers must complete and submit forms to verify eligibility. The state assesses income, household size, and other factors each year to confirm continued eligibility for Medicaid.
Given the scope of Unwinding, experts feared that hundreds of thousands in Illinois—and millions nationwide—could wrongly lose healthcare coverage. Wrongly losing coverage can compromise health – for instance, making it impossible to fill a needed prescription, or needing to cancel or postpone what should be a covered doctor’s appointment.
To address these issues, our teams worked closely with clients to help them maintain health coverage. We accepted referrals from health partners and we monitored state communications on Medicaid policy changes to keep stakeholders informed.
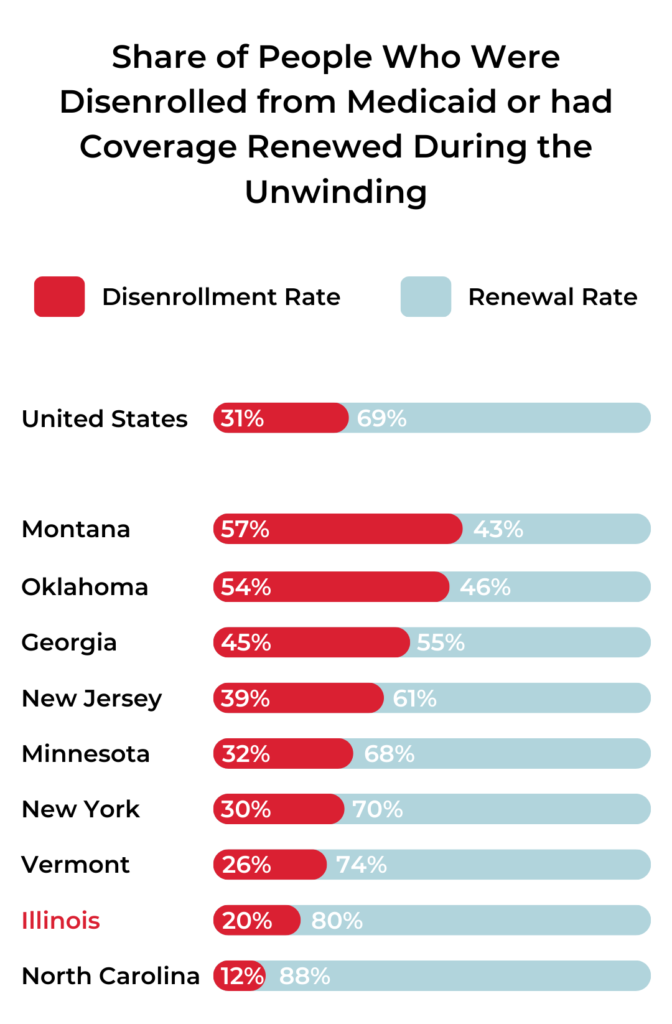
We have new data from the Medicaid Unwinding process, and we’re pleased to report positive developments through May 2024. KFF recently analyzed the unwinding and found that while 25 million people lost Medicaid coverage, 10 million more are enrolled than before the pandemic. In Illinois, the disenrollment rate was one of the lowest at 20%, and enrollment is now 14.7% higher than before COVID-19. This means more people have the essential Medicaid coverage that they are eligible for. Medicaid coverage helps us all remain healthy and live to our fullest potential.
Illinois’ Unwinding success to date stems from the hard work and foresight of the Illinois Department of Healthcare and Family Services (HFS), and their dedication to listening to and supporting advocates and community members. We at Legal Council, including Senior Staff Attorney Meghan Carter (she/her) and Deputy Executive Director of Programs and Policy Carrie Chapman (she/her), with our partners from many organizations including the AIDS Foundation Chicago, Shriver Center, EverThrive IL, Heartland Alliance, IPHCA, and Cook County Health, advocated for and supported HFS in pursuing Medicaid policy changes that help individuals maintain uninterrupted coverage. We look forward to continuing to partner with HFS to make positive change so our communities can thrive.