Service Guidelines: For Young Children with Elevated Blood Lead Levels
Funding support provided by Illinois Council on Developmental Disabilities and the Illinois Children’s Healthcare Foundation
Table of Contents
- Introduction
- Section 1: Medical effects of lead exposure
- Section 2: Developmental outcomes of low level lead poisoning in children
- Section 3: Lasting effects of childhood lead exposure
- Section 4: Supporting the Child's Development
- Section 5: Early Literacy
- Section 6: Building Parent Capacities
- Section 7:Early Intervention statutory obligations under Individuals with Disabilities Education Act (IDEA)
- Section 8: Potential effects of lead exposure on young children in the school setting
- Section 9: Lead Evaluation and Testing
- Section 10:Illinois Department of Public Health and local health department obligation reference table
- Section 11: Basic efforts to reduce lead hazards in the home
- Section 12: Lead in Water
- Section 13: Understanding the Rights of Tenants
- Section 14: Nutrition Guidelines for Families and Providers
- Glossary
Introduction
Given that low level lead poisoning has been shown to cause deficits in cognitive and behavioral development, children who have been identified to have a confirmed elevated blood lead level (EBLL) between the ages of birth to three are eligible to receive Early Intervention (EI) services. These children and their families can benefit from a continuum of targeted intervention services, from the earliest time possible, addressing development not only as deficits arise, but also in anticipation of future deficits in order to mitigate the long-lasting damage caused by early childhood lead exposure.
Low level lead exposure has irreversible effects on a child’s brain, on developing neurons, and ultimately on the ability to learn. While young children who have been lead-exposed may be asymptomatic initially, harmful effects will often become apparent later in life. Additionally, children’s brains are able to compensate and correct damage from lead more effectively the younger they are. Therefore, it is imperative that caregivers intervene early to mitigate any potential negative effects before they become apparent later in the child’s schooling years. Taking proactive measures to ensure proper development in young children who have confirmed elevated blood lead levels (EBLLs) ≥ 5 µg/dL (also written as mcg/dL, both of which mean “micrograms per deciliter”) should be the
primary focus of EI providers. Per the Centers for Disease Control and Prevention, “Although there is no empirical basis for recommending interventions with specific characteristics for children with neurodevelopmental problems resulting from an EBLL, it is reasonable to hypothesize that such children would benefit from the types of interventions shown to be effective in facilitating the neurodevelopment of other groups of children with idiopathic neurodevelopmental problems.[i] Programs in which participation begins prior to age 3 or those that include procedures to foster both child development and parenting skills may be most effective.”
Senate Bill 155 SA 1, which provides automatic eligibility for Early Intervention services to children who have been exposed to toxic substances, including lead (resulting in a confirmed EBLL ≥ 5 µg/dL), was adopted into the enrolled budget implementation bill and signed into law as part of Public Act 101-0010 on June 5, 2019. Next steps include rulemaking through DHS to update 89 Ill. Admin Code 500 Appendix E to expand the list of Medical Conditions Resulting in a High Probability of Developmental Delay to include lead poisoning. Implementing rules will be finalized by July 1, 2020.
Section 1: Medical effects of lead exposure
Despite the removal of lead from paint in the 1970s, lead-based paint remains present in homes and buildings where proper lead abatement has never been pursued. The lead dust generated from pre-1978 contaminated paint remains the largest contributing source of lead poisoning in Illinois children and can be found primarily on windowsills, doorframes, and porch decks. Children can also be exposed to lead in water, soil, consumer products, and imported foods and supplements. Lead can either be ingested orally or inhaled. Young children are particularly prone to lead exposure because they are actively exploring their environments and engaging in hand-to-mouth behavior, making them more likely to be exposed to lead by ingesting or inhaling paint particles and dust from chipped or peeling paint.
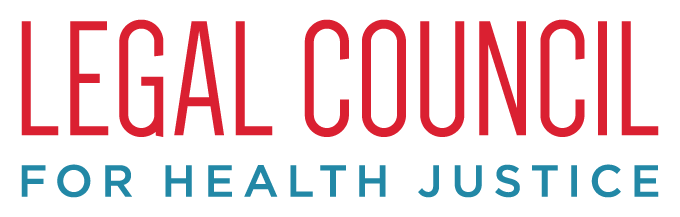
Beyond initial exposure, children are more prone to the harmful effects of lead because their bodies process lead differently than adults. Following ingestion, children can absorb into the bloodstream up to 70 percent of the lead that is in the GI tract, compared to adults who can only absorb about 20 percent. Once lead is absorbed into the body, it is distributed among blood, soft tissues, and mineralized tissues. Some of the lead is then excreted, but children retain about 50 percent of lead that enters the body, as opposed to adults who only hold on to about 1 percent. Finally, children have an immature blood-brain barrier, which means that lead molecules circulating in the blood can more easily cross from the blood to the brain where it can impact the developing nervous system.
While the harmful effects of lead exposure can be observed throughout the body, lead exposure has three main impacts on the body. Exposure to lead can:
- Interfere with the production of red blood cells, affecting the delivery of oxygen throughout the body.
- Impair kidney function.
- Inhibit development of the brain and other parts of the nervous system – an effect that can be irreversible and especially harmful to children as further discussed in Section 3: Lasting Effects of Childhood Lead Exposure.
Want to learn more? Watch Understanding the Neurocognitive Effects of Low-Level Lead Poisoning, a short video for medical providers.
Decreased academic achievement
Source
Decreased IQ
Source
Decreased performance on specific developmental measures
Source
Impaired: speech, hearing, fine & gross motor skills
Source
Increased ADHD and behavioral disorders
Source
Reading Readiness
Source
Decreased Brian Volume
Source
Increased cognitive decline later in life
Source
Section 3: Lasting effects of childhood lead exposurexi
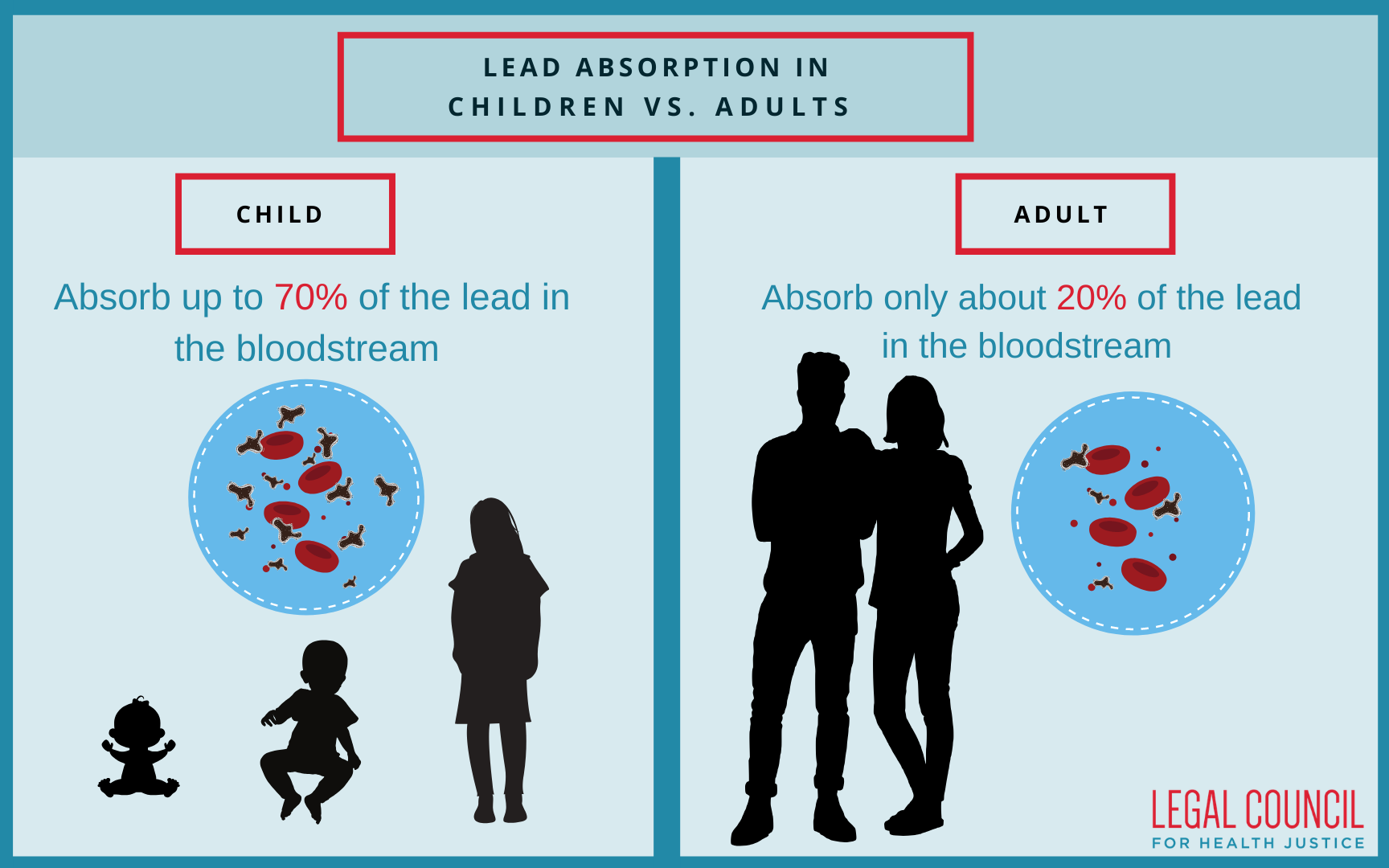
In addition to the initial health and behavioral risks to children associated with lead poisoning, there are also considerable long-term individual and societal costs. Affected children may exhibit little to no developmental delays early in life only to find themselves at a disadvantage in relation to their typically developing peers later on. Children with a history of low-level lead exposure (meaning BLL's <10 mcg/dL and in many cases even less than 5 mcg/dLmay struggle as the demand for self-regulation, attention, and higher levels of executive functioning increases with age. Unfortunately, lead poisoning disproportionately affects low-income minority individuals and therefore may be considered a significant contributor to the achievement gap in the United States.
As described in the figure, lead poisoning is a significant risk factor for neurodevelopmental deficits throughout life, and thus, children with confirmed EBLLs should be considered for and treated through Early Intervention services in anticipation of and to help prevent long-term developmental issues.[xii]
Ongoing developmental surveillance and direct service support is crucial for these children, and should not be stopped even in response to a decrease in a child’s BLL, as the level of lead in the blood does not necessarily reflect the total amount of lead in the body for children with a known history of lead exposure. It is therefore of the utmost importance that EI providers collaborate to frame their support anticipatorily and proactively in order to assess and mitigate current and future developmental concerns, sometimes years before they manifest.
Section 4: Supporting the Child’s Developmentxiii
Lead poisoning can have a broad range of developmental impacts on young children. Early Interventionists can combine their knowledge of development with evidence-based practices for fostering development to enhance families’ capacity to better support their child with an EBLL. Sections 4-6 of the Service Guidelines provides information on supporting child development and increasing parent capacity to improve outcomes for young lead-exposed children.
The first three years of a child’s life are critical for development. It is a time of rapid cognitive, social-emotional, motor and language development. In fact, between birth through age three years, 700 to 1000 new connections between cells in the brain are formed each second, making high quality, reciprocal early experiences incredibly important. Research tells us that it is both the environment, as well as early experiences, that stimulate the child’s brain to respond in either a positive manner to build a strong foundation for development or in a disruptive way to create a greater risk for developmental delays later in life.
Given what we currently know about the effects of EBLLs on developing brains, EI providers should take proactive measures to strengthen the cognitive development and social-emotional capabilities of infants and toddlers with confirmed EBLLs.
Research shows some of the best ways to support and strengthen developing brains is through sensitive, predictable and responsive caregiving relationships and positive experiences with caregivers and other important adults in children’s lives. Continuing practices that support families and caregivers in fostering their child’s development to improve cognitive functioning in areas such as attention, memory, problem solving, perseverance, self-esteem, motivation and self-control go hand in hand with promoting academic achievement and behavior regulation later in life.
Although children with EBLLs are at greater risk of developing delays, they are not likely to manifest until the child is school-aged. However, we know that Early Intervention is key to both addressing present delays and ameliorating future ones. Early Interventionists can support the child and family proactively through providing services and parent coaching that aims to keep a child on track developmentally. This service provision is similar to the types of services provided to children who are deemed eligible by being “at risk” of developmental delay or children with Down Syndrome referred to EI before the onset of delays. For additional support in service planning, including support for caregivers, see the resources listed below.
Key resources to help with the assessment and intervention planning for children with confirmed EBLLs and their families:
This 16-page guide from the Center on the Developing Child at Harvard University describes a variety of activities and games that represent age-appropriate ways for adults to support and strengthen various components of executive function and self-regulation in children.xiv
Want to learn more?
These videos are for families.
Section 5: Early Literacy
Children’s books can be very useful tools to help parents promote their child’s development. Studies have shown that when parents interact with their children around a book, there is more turn-taking (serve and return interaction), and more use of complex syntax and vocabulary than during routine daily interactions. As a result, by the age of 2 years, children who are read to regularly display greater language comprehension, larger vocabularies, and higher cognitive skills than their peers.xviii The advantage from early shared reading has been shown to persist into the elementary school yearsxix and is particularly important for lead-exposed children, who have been shown to have poorer developmental and academic outcomes.
But it’s not just the amount of reading that is important. When families read in an interactive way (e.g. asking open-ended questions, relating the book to the child’s life, giving feedback), children’s language skills improve significantly.xx In addition, diversifying the types of books families read together will offer them new opportunities to engage with reading, literacy, and with each other, allowing them to connect in ways that go beyond reading the story itself. In fact, simple board books make great imaginary play items! For example, you can help the parent and child to incorporate books into imaginary play by suggesting that they read the book to stuffed animals for a story time. Alternatively, you may suggest that the child can make up their own story about what they think is happening in a book and share it with the family for a unique experience that allows for the child to think creatively and helps them connect to a story on a more personal level.
In addition, when children do read aloud, they tend to focus more on labeling and describing pictures, rather than the more beneficial interactive reading style.xxi Encouragingly, training parents in dialogic reading has been shown to be a successful intervention.
Helpful early literacy resources
Click each header to expand.
Reach Out and Read (ROR) is a national organization that promotes literacy in pediatric offices. More than 5,800 clinics participate, serving 4.7 million children annually. Over 15 peer reviewed studies show that when children go to health clinics with Reach Out and Read Programs, their parents read more frequently with them, and their language skills are significantly more advanced.
Examples of valuable ROR resources:
- EITP Webinar on ROR “Books Build Better Brains: Promoting Language and Literacy Development in At-Risk Children”
- What Children Like in Books
- How to Raise a Reader

Section 6: Building Parent Capacitiesxxii
A child’s development is impacted by genetics as well as early experiences. Rich learning opportunities as well as stressful life circumstances and exposure to environmental toxins all shape how the brain and body of a child develops. Children develop within an environment of relationships that begins with their family and other important adults in their lives. Research has shown that the quality of parental and caregiver responsiveness is associated, in general, with developmental outcomes for children.
Accordingly, another key component in the service provision of children with EBLLs should focus on building parent capacities through active skill building by way of practice and engagement with children and coaching by the EI provider. It is by this process that parents build the skills they need in order to nourish and shape the healthy development of their children. In doing so, the children of these families will be better equipped to overcome the potential for negative developmental outcomes that can present as a result of their EBLLs.
Early Intervention providers are encouraged to access the following resources to enhance parent capacities:
- Family Capacity-Building Practices Checklist: This checklist includes practices for engaging parents and other family members in using child-level interventions to promote child learning and development in ways that strengthen parenting confidence and competence.xxiii
- DEC Recommended Practices: Early Intervention providers are encouraged to use the DEC Recommended Practices F1-F10 (pp. 16-19) related to family practices to help guide their work in building capacities in the families of children with confirmed elevated BLLs.xxiv
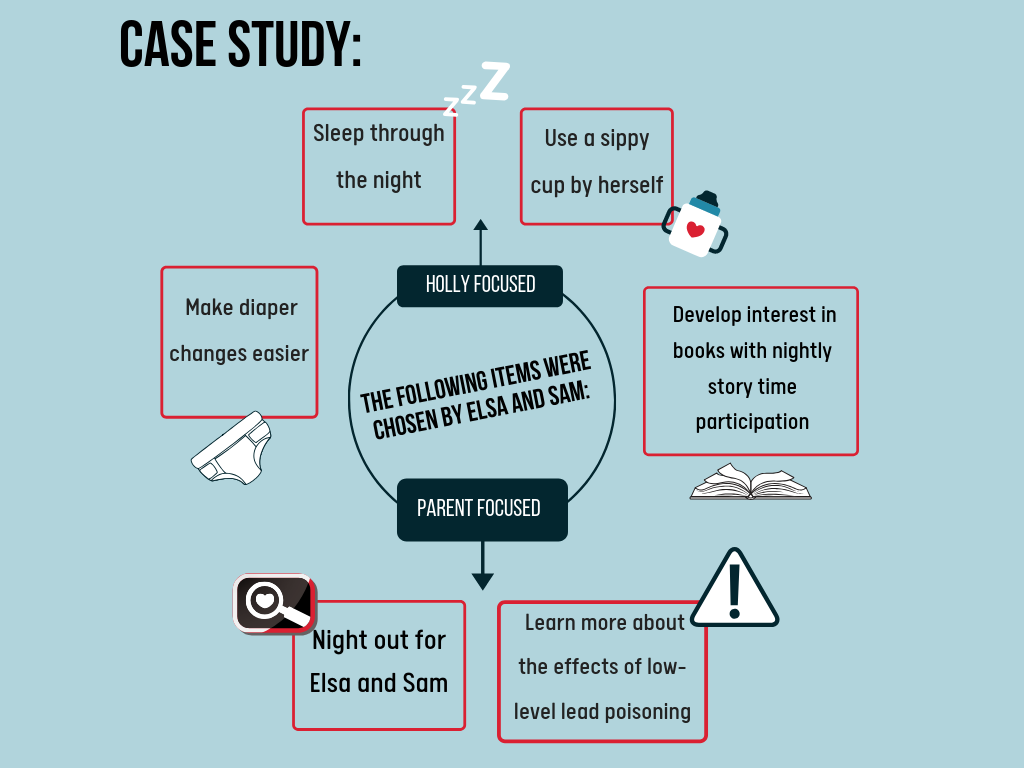
A Case Study: Holly’s Story
Below is a case study that presents a proactive strategy to Early Intervention services.
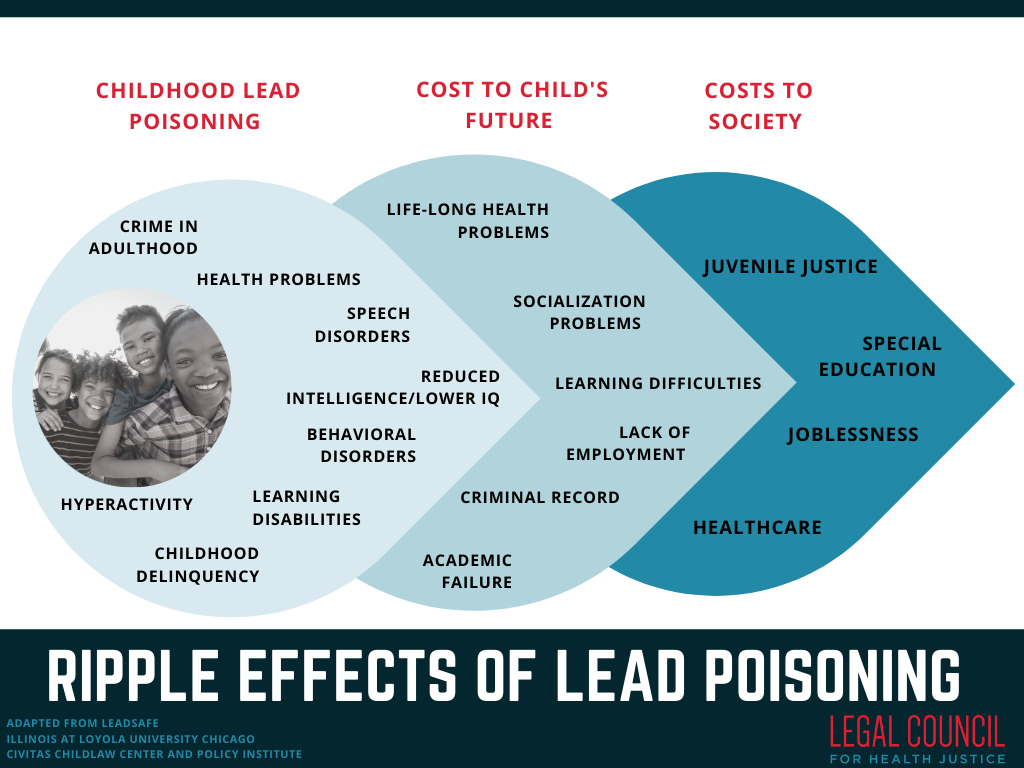
Holly is a 20-month old girl, who was referred to Early Intervention by her pediatrician after a confirmed elevated blood lead test obtained at her 12 month well-child visit. After meeting with Annabelle (their service coordinator), Holly’s parents, Elsa and Sam, reported that even though she was not showing delays, they still had questions about her development. Annabelle explained that Holly would qualify for Early Intervention based on her medical diagnosis of a confirmed blood lead level of 5µg/dL. Annabelle also explained that even if Holly is not showing delays, she and her family can still get support from Early Intervention.

Following the interview, Holly was evaluated by a Developmental Therapist and an Occupational Therapist – this was decided by Annabelle based on the information that Elsa and Sam reported during the Routines-Based Interview.
The Occupational Therapist and Developmental Therapist went out separately and sent in their reports to Annabelle. The results showed that Holly was currently not experiencing any delays in her development; however, she was still eligible for Early Intervention based on her EBLL diagnosis. A couple of weeks later, the IFSP team convened to develop an Individualized Family Service Plan.
Annabelle began the IFSP development meeting by having everyone introduce each other, as this was the team’s first time coming together. After introductions, Annabelle reviewed the evaluation and assessment information, giving Elsa and Sam an opportunity to ask questions after each section she explained. Annabelle made sure to turn her computer screen while entering the information about present levels of development so Elsa and Sam could see what was being written, frequently double-checking with Elsa and Sam to make sure that the information was accurate. During this process, she encouraged everyone on the team to give input. After filling in the information that Sam and Elsa provided about Holly’s health history, Annabelle started to review the list of priorities they had made together following the RBI during their first visit. Going through the list one-by-one, Annabelle asked if each item was something that Sam and Elsa wanted to work on. She found this to be much easier than coming up with things out of the blue. Although Elsa and Sam had initially listed 10 priorities during their IFSP meeting, they decided during their IFSP meeting to focus on 6 of the items.
Annabelle asked Elsa and Sam many questions about the items. These outcomes were developed together as a team:
- Holly will participate in story time by sitting and not running away, and pointing to objects in the book in order to learn new words and continue to develop her language skills
- Holly will use a sippy cup to drink liquids so that she can stop using the bottle
- Elsa and Sam will establish a bedtime routine so that Holly can sleep through the entire night
- Holly will tolerate diaper changes and not run away in order to get her diaper changed and stay in place during this activity
- Elsa and Sam will learn about the connection between low-level lead poisoning and developmental delay within 3 months
- Elsa and Sam will have one monthly date night
Once the outcomes were developed, Annabelle asked Elsa, Sam, and the rest of the team to think about strategies that could help Elsa and Sam reach their goals. After some thought, the support and services that would help Elsa and Sam meet their outcomes were developed and consented to by the team. The IFSP team decided the Developmental Therapist would support the child and family outcomes by visiting Holly and her parents twice a month for three months, then reducing the frequency to once a month as appropriate. The Occupational Therapist would also consult as needed, particularly on using a sippy cup and tolerating diaper changes. Annabelle reviewed all the outcomes and strategies, ensured understanding and agreement amongst all team members, and proceeded to have Sam and Elsa sign their agreement with the plan.
Proactive Strategy: Key Takeaways from Holly’s Story
- Building a relationship with the family to better understand how they understand their child’s development and any goals they have for their child and family;
- Working with the family to establish culturally and developmentally appropriate practices that promote the child’s development within the context of the family’s daily routines;
- Co-creating a plan with the family to meet their identified goals;
- Using typical EI strategies to center the child in their family unit and supports parent capacity through developmentally informed coaching from the interventionists.
IDEA Part C enumerates Early Intervention Services as those services falling under these categories:
- family training, counseling, and home visits
- speech-language pathology and audiology services, and sign language and cued language services
- physical therapy
- service coordination services
- early identification, screening, and assessment services
- social work services
- health services necessary to enable the infant or toddler to benefit from the other early intervention services
- special instruction
- medical services only for diagnostic or evaluation purposes
- psychological services
- occupational therapy
- assistive technology devices and assistive technology services
- vision services
- transportation and related costs that are necessary to enable an infant or toddler and the infant's or toddler's family to receive another service described in this paragraph
Furthermore, these services are to be delivered by qualified personnel, including:
- Family Therapists
- Speech-language Pathologists
- Audiologists
- Physical Therapists
- Nurses
- Social Workers
- Registered Dietitians
- Special Educators
- Developmental Therapists
- Pediatricians and other physicians
- Psychologists
- Occupational Therapists
- Orientation and Mobility Specialists
- Vision Specialists, including Ophthalmologists and Optometrists
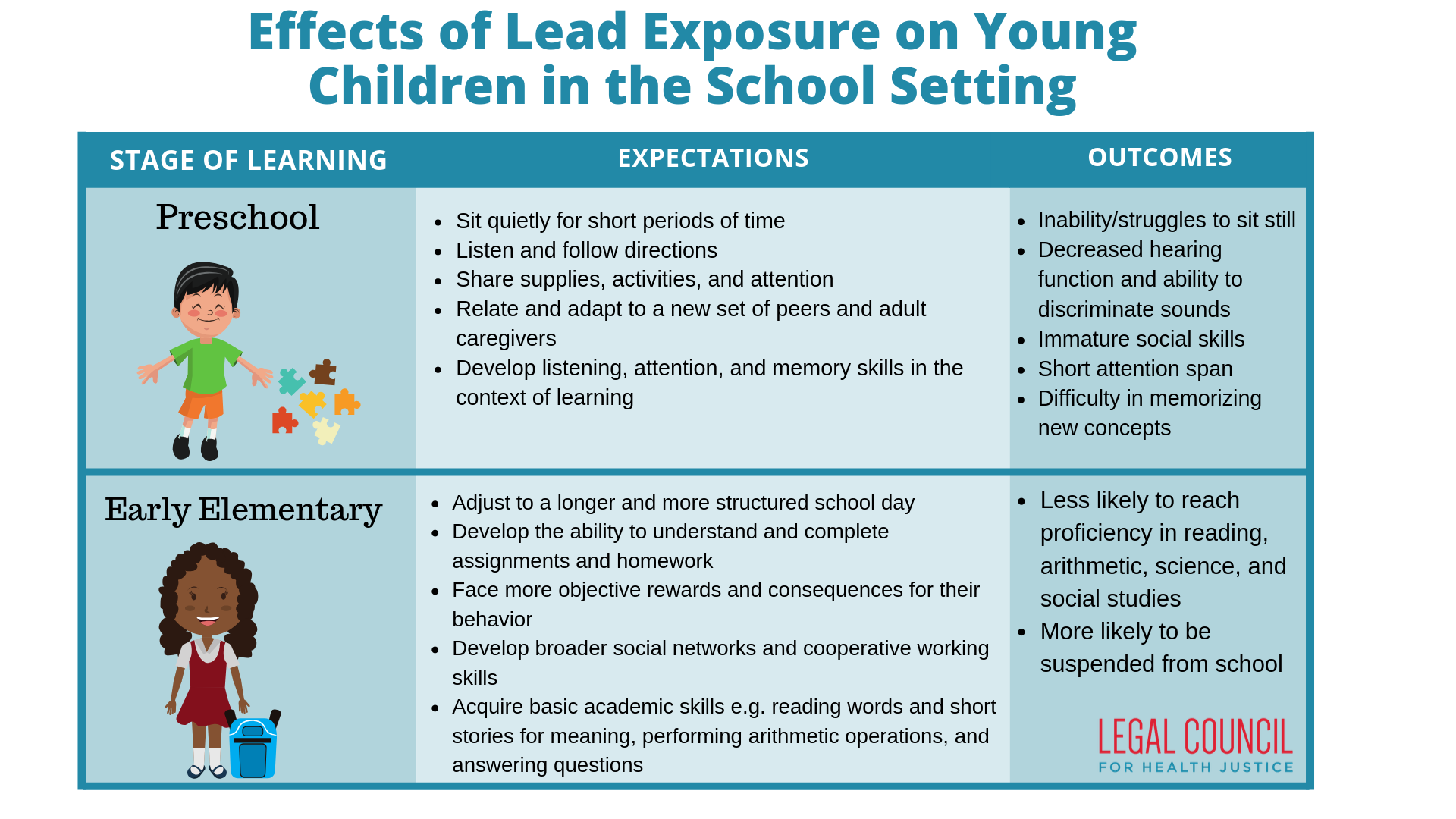
Section 8: Potential effects of lead exposure on young children in the school settingxxvii
The table below juxtaposes a sample of expectations in early childhood learning settings for typically-developing children with education-specific challenges associated with lead exposure. This can be a useful tool when considering possible areas to support a lead-exposed child in order to foster school readiness.
Click image to enlarge.
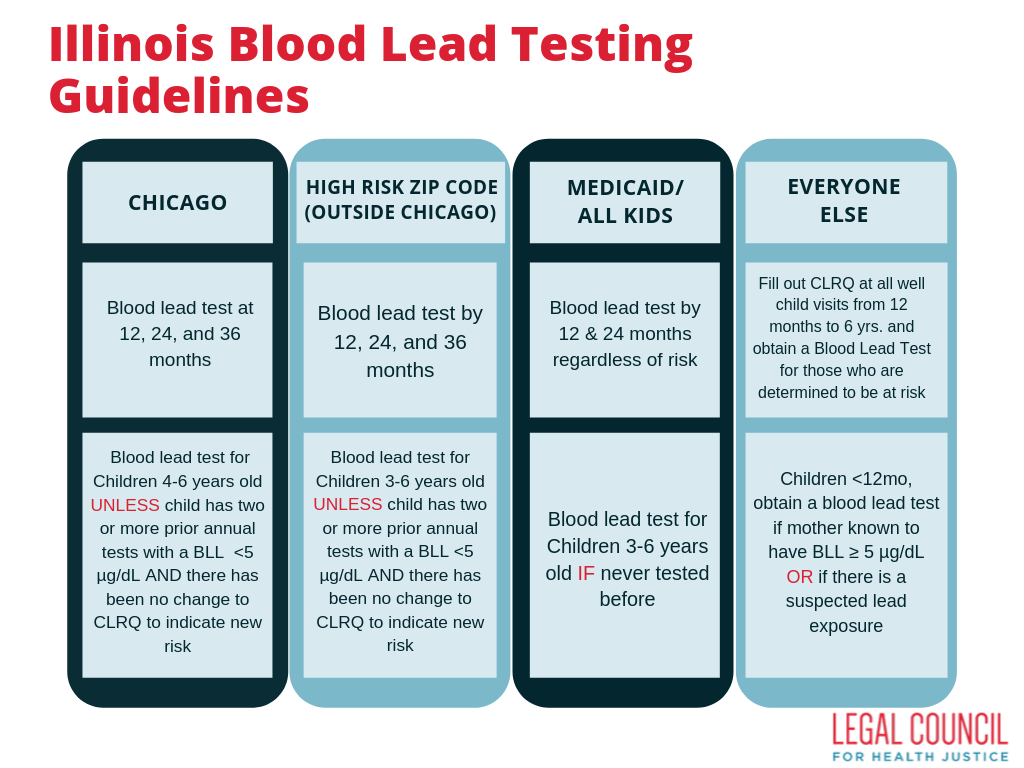
Section 9: Lead Evaluation and Testing
Medical providers should conduct lead screening at annual well child visits from 12 months to 6 years. At minimum, this requires a family to complete the Illinois Childhood Lead Risk Questionnaire (CLRQ) to determine if a child is at risk of lead exposure. If a child is determined to be at risk based on the CLRQ, their zip code (high risk zip codes are listed on back side of CLRQ), or their insurance status blood lead testing is required. The chart to the left describes the blood lead testing guidelines that are recommended by the Illinois Department of Public Health Lead Program. Note that when a child falls within multiple categories (for example a patient lives in Chicago AND is on Medicaid/All Kids), the child should receive whichever guideline requires more blood lead testing. When a child has a history of an elevated confirmed blood lead level ≥ 5 µg/dL additional follow-up testing is necessary to ensure that the child’s lead level decreases (this is not reflected in table).
Of note, any child between the ages of 6 months and 6 years is required to provide certification from a medical provider that he or she has been tested or screened prior to admission to any licensed child care center or facility including any home-based child care program, nursery school, preschool, Head Start program, kindergarten, or elementary school. Also, any sibling of a child who has been identified to have an elevated blood lead level should be referred for blood lead screening.
For complete information about lead evaluation and testing see the Childhood Blood Lead Evaluation and Testing Recommendations from the IDPH.
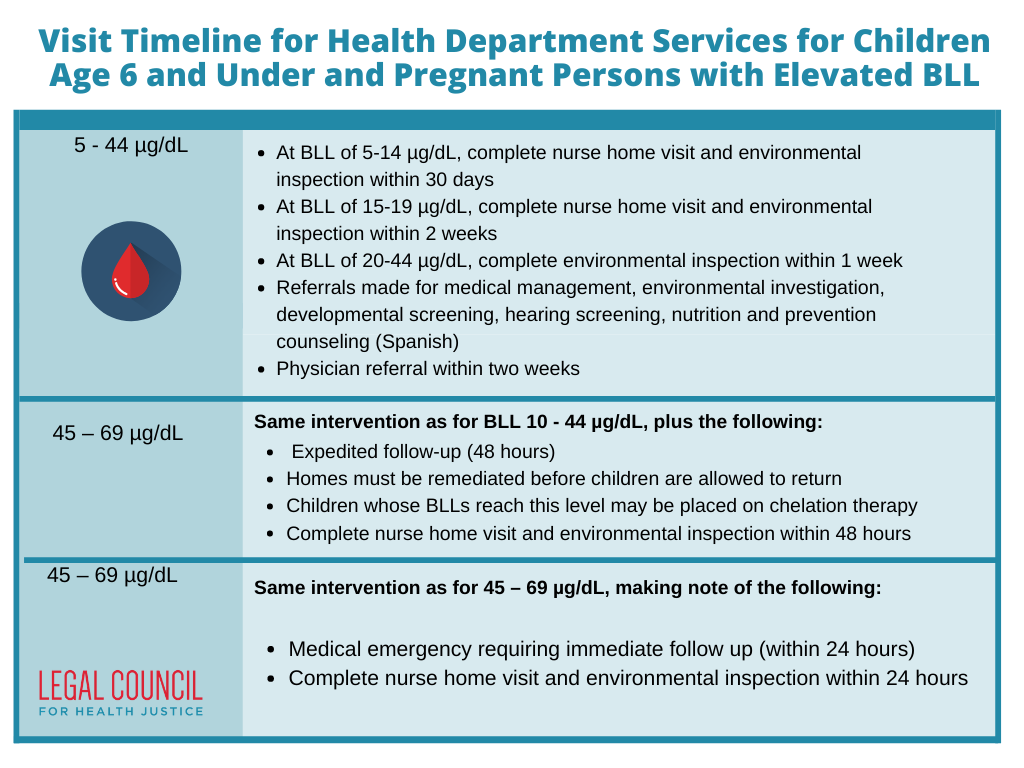
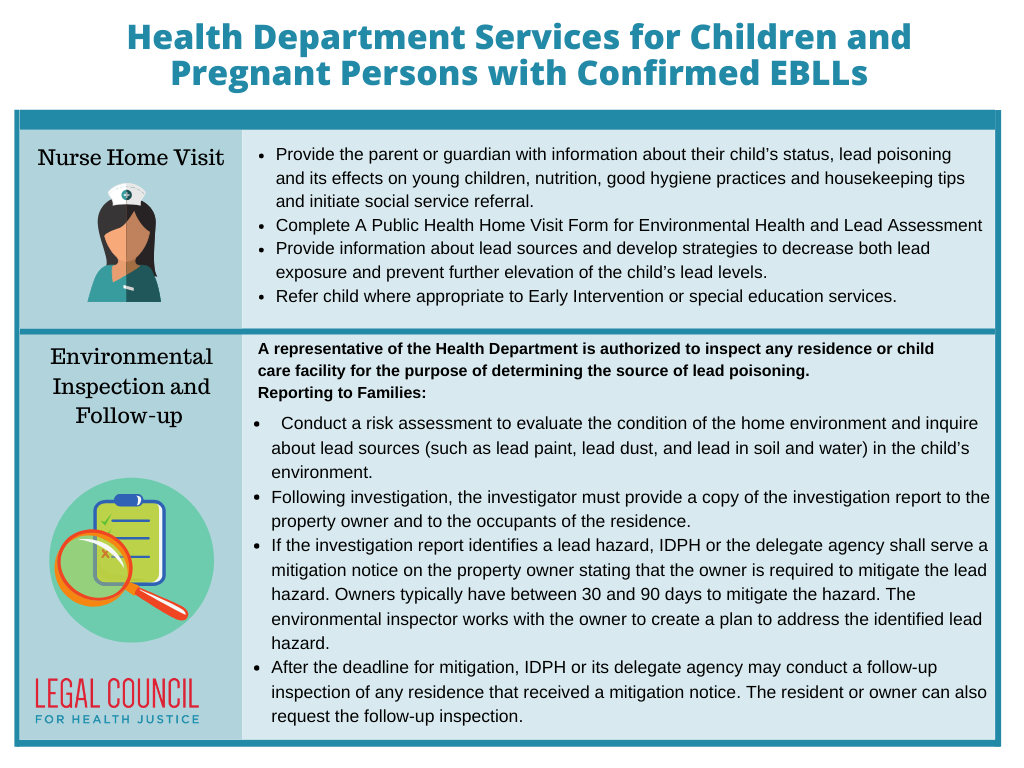
The purpose of this section is to assist EI providers and others serving children with confirmed elevated blood lead levels (EBLLs)xxx by providing an overview of the duties and responsibilities of IDPH Delegate and Non-Delegate Agencies in their support of children with EBLLs and their families. The table below summarizes agency responsibilities in the process of testing children for EBLLs, managing cases, educating families, and providing environmental inspection and mitigation. In accordance with Public Act 100-0723, Illinois’ Blood Lead Reference Level (BLL) was moved from 10 to ≥ 5 µg/dL as a best practice, in line with the CDC’s current reference value. In addition, IDPH has adopted rules that define EBLLs as a venous confirmed blood lead level greater than or equal to 5 μg/dL. Therefore, just a capillary finger prick test is not sufficient, and blood lead levels must be obtained by a venous blood draw in order to be considered a confirmed EBLL which triggers a public health nurse home visit and environmental home inspection. Public Act 101-0010 adopts this same standard for automatic EI eligibility. As such, all children referred for Early Intervention services should also receive a public health nurse home visit and environmental home inspection.
For more information about delegate agency responsibilities see the Guidelines for Local Health Departments.
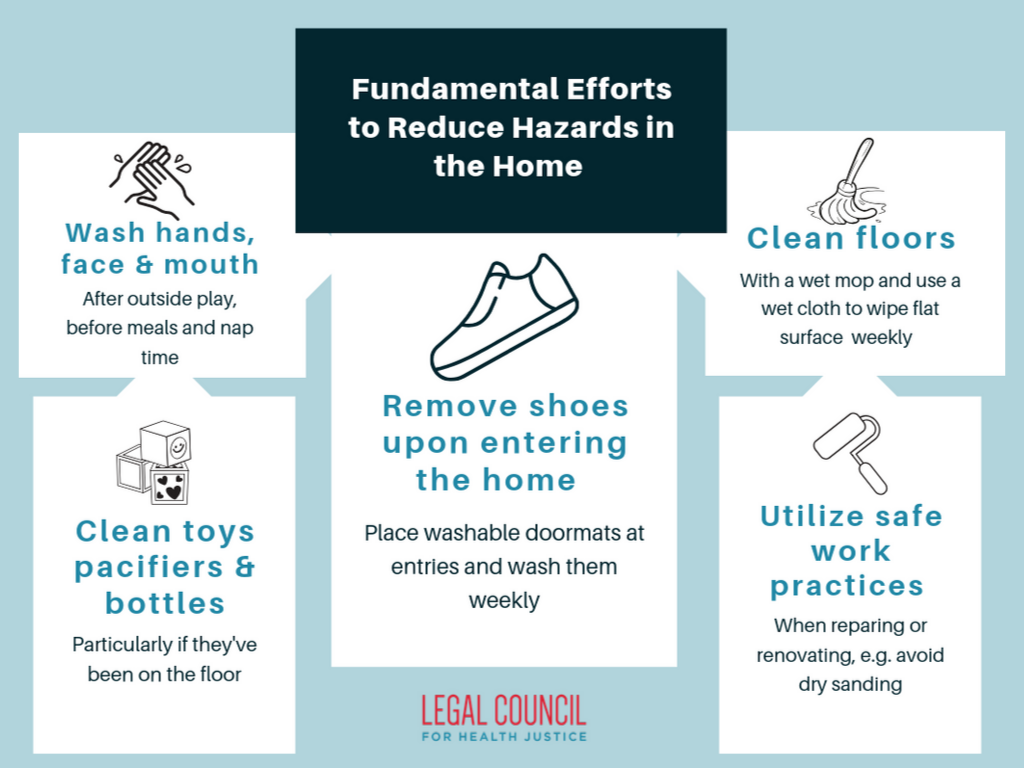
Section 11: Basic efforts to reduce lead hazards in the homexxxi
For families living in high risk zip codes and/or housing constructed prior to 1978, the following steps can be taken to reduce lead hazards in the home:
- Renters should notify landlord of peeling or chipping paint
- Clean floors, window frames, window sills, and other surfaces weekly. Use a mop, sponge, or paper towel with warm water and a general all-purpose cleaner.
- Thoroughly rinse sponges and mop heads after cleaning dirty or dusty areas.
- Wash children's hands often, especially before they eat and before nap time and bedtime.
- Keep play areas clean. Wash bottles, pacifiers, toys, and stuffed animals regularly.
- Ensure that children are not chewing on materials found at playgrounds, as older play equipment and artificial turf may contain lead.
- Keep children from chewing window sills or other painted surfaces.
- Clean or remove shoes before entering your home to avoid tracking in lead from soil.
- Housekeeping Tips to Reduce Lead Exposure in English and Spanish.
- Make sure children eat healthy and nutritious meals as recommended by the National Dietary Guidelines and discussed in Section 14: Nutritional Guidelines for Families and Providers. Children with well-balanced diets should absorb less lead. More information about nutrition and lead poisoning here and in Spanish too.
- Families should stay up-to-date on current recalls on children’s products. They can visit the Consumer Product Safety Commission to review the latest updates.
Additional resources: When to Have Your Child Tested For Lead, Sources of Childhood Lead Poisoning from IDPH in English and Spanish, Preventing Childhood Lead Poisoning from the CDC, and IDPH resources on Intervention in English and Spanish.
If gardening in an area with possible lead contamination either:
- Use raised planting beds, OR
- Separate new planting soil from contaminated soil by placing a thick layer of compost or mulch over contaminated soil, placing landscape fabric on top of the mulch or compost, and placing new clean soil to plant in on top of the fabric.
- Prevent children from playing on bare soil, and if possible, cover it with mulch or grass.
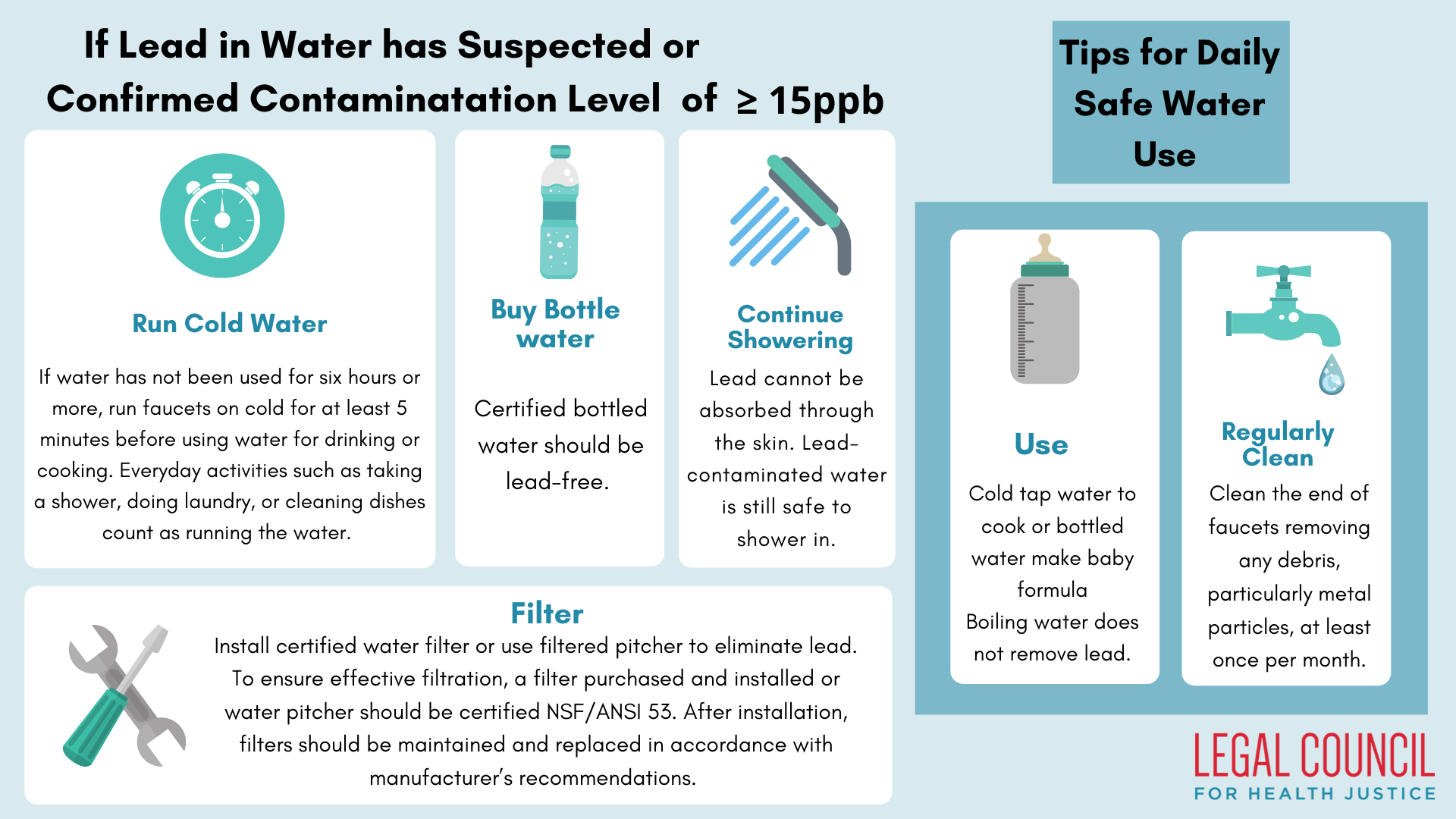
Lead poisoning can occur through the consumption of lead-contaminated water. This contamination is typically caused by the corrosion of pipes and other fixture materials within residences or public water systems. Measures including EPA’s Safe Water Drinking Act, EPA’s Lead and Copper Rule, and amendments to Illinois Lead Poisoning Prevention Act PA 099-0922, have sought to reduce the quantity of lead in public water supplies.
Keep in mind that lead in water is going to affect children differently depending on their age. For example, relatively immobile infants that consume most of their diet in liquid form (as reconstituted baby formula) will be particularly vulnerable to lead poisoning via water. Consequently, special attention should be paid to children in this category. On the other hand, mobile children exploring the world with their mouths are likely to be more susceptible to lead via dust or paint. However, remember that lead in all forms is hazardous to children of all ages.
Below are helpful tips to share with families for handling potentially contaminated water sources:
- Check Consumer Confidence Reports (CCR): Contact the local water authority to request a CCR which will provide results of the most recent water report.
- Get tested: Contact state lead programs for information about water testing. In Chicago, water testing is free and can be ordered at Chicagowaterquality.org.
- Ask the age of the home: Lead service lines were banned in 1986, so risk is highest in homes built prior to 1986
- Provide a copy of Lead in Drinking Water Fact Sheet.
Long-term Strategies:
- Hire a licensed plumber to determine whether plumbing materials such as fixtures, piping, fittings, and service lines contain lead. If lead is identified, replace plumbing materials with lead-free materials approved under the Illinois Plumbing Code.
- Prioritize replacement of fixtures by frequency of use for cooking, drinking, and making baby formula.
- Even after replacement, always follow best practices.
Section 13: Understanding the Rights of Tenants
Moving in:
- Property owners and landlords with property built before 1978 are required to disclose to prospective buyers and tenants all information concerning the existence and location of lead-based paint hazards, including all records and reports concerning lead-based paint and/or lead-based paint hazards.
- Property owners and landlords are required to provide tenants or buyers with information on lead hazards, typically, a copy of the EPA-approved booklet “Protect Your Family From Lead In Your Home.” They are also required to include language in the sale or rental agreement confirming that the seller or landlord has complied with all notification requirements.
- If a unit has a mitigation notice, the landlord cannot rent to a new tenant prior to proper mitigation.
Tenants’ Right of Inspection:
- Tenants living in public housing or subsidized housing have a right to the inspection and control of lead hazards as part of initial and periodic inspections conducted by the public housing authority.
If lead is found in a home:
-
The Public Health Department will provide a copy of the investigation report to the property owner and tenants and a mitigation notice to the property owner. The mitigation notice requires the property owner to fix the lead hazard and tells the owner how long they have to fix the hazard (no more than 90 days). The property owner is required to notify all tenants of any proposed lead remediation work and the environmental inspector works with the owner to create a plan to address the identified lead hazard.
If a property owner won’t address a lead problem:
- Tenants who do not feel their property owner is properly addressing the lead hazard should call their local or state public health department and consider enlisting the assistance of their medical provider.
- Tenants in Illinois can also call the Metropolitan Tenants’ Organization at (773) 292-4988 between 1:00 and 5:00 p.m., Monday through Friday.
Health Department Reporting Contacts:
- Illinois Department of Public Health’s Environmental Lead Program (if you don’t know how to contact local health department):
- Phone: 217.782.3517, or 866.909.3572
- Chicago Department of Public Health Lead Poisoning Prevention Program
- Phone: 312.717.5323(LEAD)
- Online
- To request a free lead test kit for tap water in the City of Chicago, call 311.
- Cook County Department of Public Health
- Phone: 708.663.8054 (between 8:30 a.m. and 4:30 p.m., Monday through Friday)
- Email: ddurica@cookcountyhhs.org
For more information, see the following resources:
- EPA HUD Fact Sheet on Disclosure of Lead-Based Paint Hazards in Housing
- “Protect Your Family From Lead In Your Home” Booklet
- Real Estate Disclosure
- Understanding Apartment Conditions and Repairs
- Understanding Inspection, Risk Assessment, and Abatement
- Healthy Homes: Keeping Your Home Healthy and Safe
Section 14: Nutrition Guidelines for Families and Providers
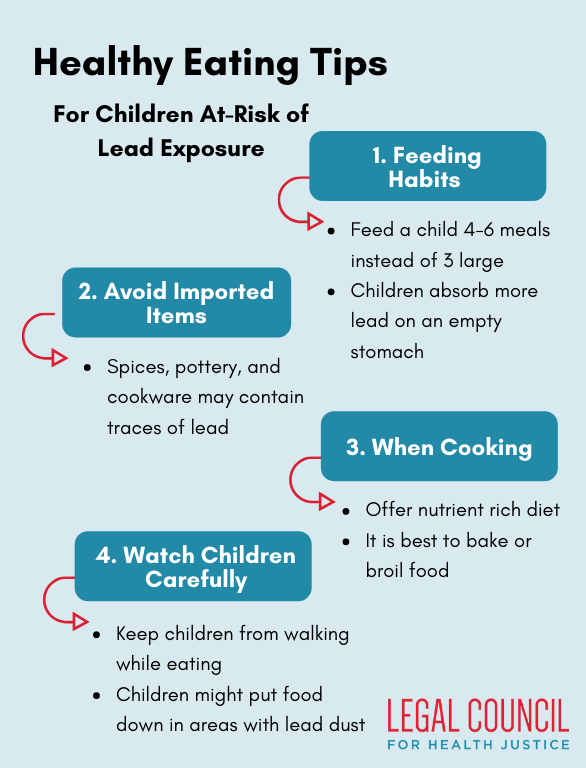
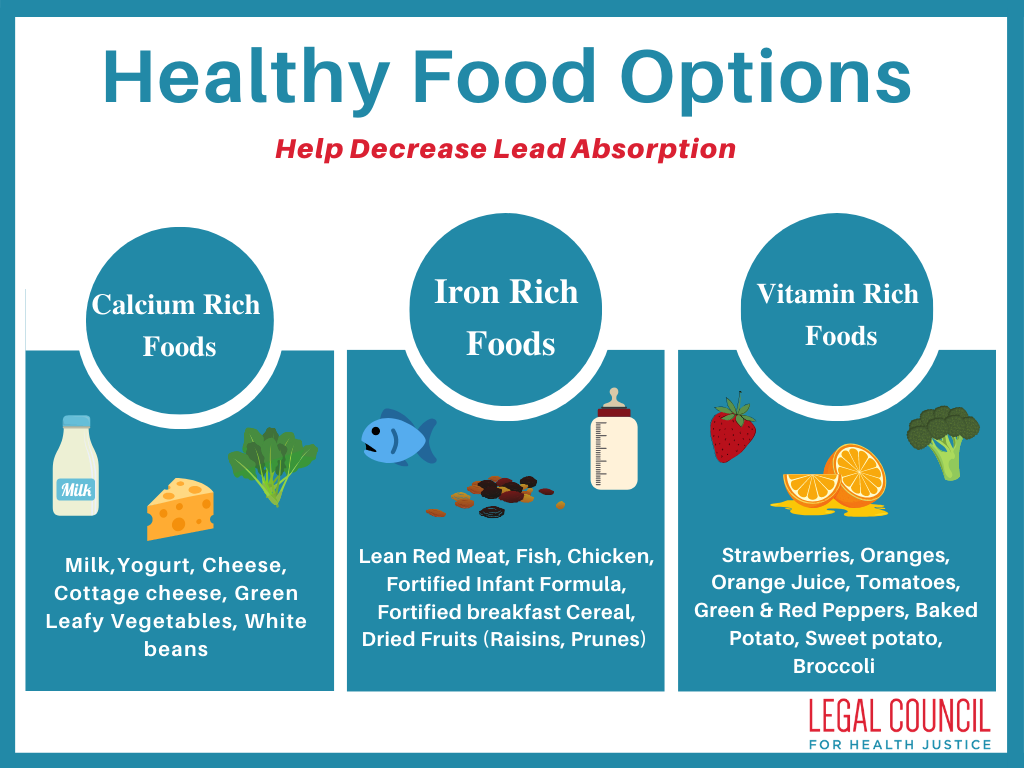
A child’s nutritional status can affect the degree of lead absorption in the body. A parent should follow the most recent Dietary Guidelines, which includes a balance of the five food groups – vegetables, fruits, whole grains, protein-rich foods and dairy products – that are the building blocks for a healthy diet. Additionally, it is important for child’s diet to be rich in calcium, iron, and vitamin C.
Importance of Cultural Competence when Discussing Nutrition with Families
Cultural competence is best defined as a set of coexisting behaviors, attitudes, and policies that come together in a system, agency or among practitioners, empowering them to work effectively and respectively with cultures other than their own. This practice is important as cultural background, language, and beliefs all inform how individuals and families perceive diagnosed medical conditions, developmental delays and the expectations of appropriate intervention. EI providers should build their capacity for cultural and linguistic competence in order to effectively deliver services that meet the cultural and linguistic needs of their patients and families. A culturally competent practice of care can not only aid in improving developmental outcomes and the quality of intervention but is essential to reducing racial and ethnic care inequities.
Additionally, it is important to note that cultural competence is a process that takes commitment to active and ongoing engagement, self-reflection, and cross-cultural experiences. Early interventionists should seek out trainings and comprehensive strategies that allow them to both acknowledge that culture is one of the many factors that influences their patients’ development, as well as provide services in a manner that is responsive to those cultural attitudes, languages and behaviors. For additional resources on cultural competence visit ECTA Preparing Personnel to Meet the Needs of Culturally and Linguistically Diverse Families and USDA Food and Nutrition Information Center Ethnic and Cultural Resources
Healthy Eating Tips for Children At-Risk for Lead Exposurexxxiv
When speaking to families about nutrition, it is important to remember that food and rituals around and related to food are often intrinsic to one’s culture – thus, recommendations should be given within a cultural context. Above and below are a few healthy eating tips for children at risk for lead exposure.
The following resources can be provided to families:
Eat.Move.Save Making Healthier Choices on a Budget: This website, run by University of Illinois Extension, is full of tips for how to eat balanced meals while on a budget. It is not specifically geared towards lead-conscious eating, but includes a database of healthy, low-cost recipes with nutritional information for each, and information on safe cooking practices and reading nutrition labels.xxxviii
Nutrition and Lead Poisoning Prevention: This web page, produced by the Nebraska Department of Health and Human Services, contains a more expansive list of recommended foods for children at risk of lead exposure.xxxix
To assist in overcoming the financial barriers to healthy eating connect families to the following programs:
- LINK Up Illinois: At Illinois Products Farmers’ Markets for each dollar up to 25 dollars spent with a LINK card, individuals will receive match coupons to spend on fruits and vegetables. Learn more and locate farmers markets through LinkUp Illinois.xl
- WIC Farmer’s Market Nutrition Program: This program provides WIC Program participants with coupons to purchase fresh fruits and vegetables at local farmers’ markets in addition to the regular WIC food package. WIC recipients can apply for the Farmer’s Market Nutrition Program at their local DHS office.xli
- AmpleHarvest: Ample Harvest has a directory of food pantries across the United States. Individuals can enter their ZIP code and locate the pantry nearest to them.xlii
- Greater Chicago Food Depository Cook County Producemobile: The Producemobile takes donated fresh fruit and vegetables directly to neighborhoods in Cook County where produce is difficult to find. Individuals can locate Producemobile drop off locations and times via the Greater Chicago Food Depository website.xliii
EI Nutrition Services
Early Intervention providers offering nutrition services to children with confirmed elevated BLLs should focus on the following:
1) Conducting individual assessments in:
- Nutritional history and dietary intake;
- Feeding skills and feeding problems; and
- Food habits and food preferences;
2) Developing and monitoring appropriate plans to address the nutritional needs of children
3) Making referrals to appropriate community resources to carry out nutrition goals
The Supplemental Nutrition Program for Women, Infants and Children (WIC)
The Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides federal grants to states to assist them in meeting the nutrition needs of low-income pregnant and post-partum women, infants, and children up to age five.xliv WIC recognizes elevated blood lead levels of 5 µg/dL or higher as a nutrition related medical risk. Therefore, lead program public health nurse case managers will likely refer the family to WIC if they fit the eligibility criteria.
You can also inform families you are serving in EI to consider WIC benefits and refer them to the WIC office to apply. Use the DHS Office Locator to find their nearest location. They can also use the pre-screening tool at https://wic.fns.usda.gov/wps/pages/preScreenTool to learn more about their potential eligibility. Individuals participating in the WIC program can receive funds to purchase healthy foods as well as information on nutrition, breastfeeding, and access to healthcare.xlv They can receive WIC in addition to SNAP and can receive benefits without providing proof of citizenship or immigration status.
Glossary
Abatement - Any approved work practices that will permanently eliminate lead exposure or remove the lead-bearing substances in a regulated facility
BLL - Blood lead level
Blood lead test - Blood lead testing by venous or capillary methodology
Capillary test - blood lead test done by pricking finger or heel. This test alone is not sufficient to be considered a confirmed elevated blood lead level that triggers case management
Case Management/Case Follow-up - Any public health activity coordinating, providing and overseeing the services required to reduce BLLs <5 µg/dL
CDC - U.S. Centers for Disease Control and Prevention
Child - A person under the age of 16
Childhood Lead Risk Questionnaire - The questionnaire developed by the IDPH for use by physicians and other health care providers to determine risk factors for lead exposure children 6 years of age or younger; any answers of “yes” or “don’t know” on the questionnaire should result in a blood lead test
Code - Illinois Lead Poisoning Prevention Code
Confirmatory - Refers to a venous blood test. This is required to provide all case management activities (public health nurse home visit and environmental home inspection) and is also necessary for eligibility for Early Intervention services.
Delegate Agency - A unit of local government or health department approved by the IDPH to carry out provisions of the Lead Poisoning Prevention Act.
IDPH - Illinois Department of Public Health
EBLL - Elevated blood lead level; a blood lead level ≥5 µg/dL
Environmental home inspection - A surface-by-surface investigation in the home to determine the presence of lead
High-risk ZIP Codes - Designated areas of the state where children 6 years of age and younger are considered at high risk for lead exposure; all children residing in a high-risk zip code must receive blood lead testing.
Lead evaluation/screening - Administration of the Childhood Lead Risk Questionnaire to the parent by a health care provider
Lead hazard - A lead-bearing substance that poses an immediate health hazard to humans
Lead poisoning/exposure - The condition of having blood lead levels in excess of those considered safe under the Illinois Lead Poisoning Prevention Act
Mitigate - The remediation of a lead hazard so that the lead-bearing substance does not pose an immediate health hazard to humans
Remediation - Reversing or stopping a lead hazard so that any lead-bearing substance does not pose an immediate health risk to humans
WIC - Women, Infants and Children Nutrition Program offered by most local health departments
Footnotes
[i] Scharf, R.J., Schard, G.J., & Stroustrup, A. (2016). Developmental milestones. Pediatrics in Review, 37(1), 25-38. http://dx.doi.org/10.1542/pir.2014-0103
[ii] Amato MS, M. S., Moore, C. F., Magzamen, S., Imm, P., Havlena, J. A., Anderson, H. A., & Kanarek, M. S. (2012). Lead exposure and educational proficiency: moderate lead exposure and educational proficiency on end-of-grade examinations. Annals of Epidemiology, 22(10), 738–743. https://doi.org/10.1016/j.annepidem.2012.07.004
[iii] Evens, E., Hryhorczuk, D., Lanphear, B.P., Rankin, K.M., Lewis, D.A., Forst, L., & Rosenberg, D. (2015). The impact of low-level lead toxicity on school performance among children in the Chicago Public Schools: a population-based retrospective cohort study. Environmental Health, 14:21. https://doi.org/10.1186/s12940-015-0008-9
[iv] Zhang N., Baker H.W., Tufts M., Raymond R.E., Salihu H., & Elliott M.R. (2013). Early childhood lead exposure and academic achievement: evidence from Detroit public schools, 2008-2010. American Journal of Public Health, 103(3), e72-77. https://doi.org/10.2105/AJPH.2012.301164
[v] Miranda M.L., Kim, D., Osgood C., & Hastings C. (2011). The impact of early childhood lead exposure on educational test performance among Connecticut schoolchildren, phase 1 report. Durham, NC: Children's Environmental Health Initiative, Duke University.
[vi] Miranda, M.L., Kim, D., Reiter, J., Overstreet Galeano, M.A., & Maxson, P. (2009). NeuroToxicology, 30(6), 1019-1024. https://doi.org/10.1016/j.neuro.2009.07.012
[vii] Lanphear, B. P., Hornung, R., Khoury, J., Yolton, K., Baghurst, P., Bellinger, D. C., … Roberts, R. (2005). Low-Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled Analysis. Environmental Health Perspectives, 113(7), 894–899. http://doi.org/10.1289/ehp.7688
[viii] McLaine, P., Navas-Acien, A., Lee, R., Simon, P., Diener-West, M., Agnew, J. (2013). Elevated blood lead levels and reading readiness at the start of kindergarten. Pediatrics, 131(6), 1081-1089. http://doi.org/10.1542/peds.2012-2277
[ix] Stefanak M., Diorio J, & Frisch L. (2005). Cost of child lead poisoning to taxpayers in Mahoning County, Ohio. Public Health Reports, 120(3), 311-315. https://doi.org/10.1177/003335490512000316
[x] Needleman H.L., Riess J.A., Tobin M.J., Biesecker G.E., Greenhouse J.B. (1996). Bone lead levels and delinquent behavior. JAMA, 275(5), 363-369. https://doi.org/10.1001/jama.1996.03530290033034
[xi] Educational Services for Children Affected by Lead Expert Panel (2015). Educational Interventions for Children Affected by Lead. Atlanta, GA: Centers for Disease Control and Prevention. Retrieved from http://www.cdc.gov/nceh/lead/publications/Educational_Interventions_Children_Affected_by_Lead.pdf
[xii] LeadSafe Illinois at Loyola University Chicago Civitas ChildLaw Center and Policy Institute. Ripple effects of childhood lead poisoning. Retrieved from http://www.leadsafeillinois.org/facts/ripple-effects.asp
[xiii] Harvey, B. (2002). Managing elevated blood lead levels among young children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta, GA: Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nceh/lead/casemanagement/managingEBLLs.pdf
[xiv] Center on the Developing Child Harvard University (2015). Enhancing and Practicing Executive Function Skills with Children from Infancy to Adolescence. Retrieved from http://46y5eh11fhgw3ve3ytpwxt9r.wpengine.netdna-cdn.com/wp-content/uploads/2015/05/Enhancing-and-Practicing-Executive-Function-Skills-with-Children-from-Infancy-to-Adolescence-1.pdf
[xv] Vroom. Retrieved from https://www.vroom.org/
[xvi] Zero to Three: Early Connections Last a Lifetime. Family, Friend & Neighbor Care. Retrieved from https://www.zerotothree.org/resources/series/family-friend-neighbor-care
[xvii] Illinois Early Intervention Clearinghouse. Everyday Early Intervention. Retrieved from https://eiclearinghouse.org/?s=everyday+early+intervention
[xviii] Raikes, H., Pan, B.A., Luze, G.J., Tamis-LeMonda, C.S., Brooks-Gunn, J., Constantine, J., Tarullo, L.B., Raikes, H.A., & Rodriguez, E. (2006). “Mother-child book reading in low-income families: Correlates and outcomes during the first three years of life.” Child Development, 77(4).
[xix] Snow, C.E., Burns, S., & Griffin. P. (1998). Preventing reading difficulties in young children. National Academy Press: Washington, DC.
[xx] Whitehurst, G.J., Falco, F.L., Lonigan C.J., Fischel, J. E., DeBaryshe, B. D., Valdez-Menchaca, M. C., & Caulfield, M. (1988). Accelerating language development through picture book reading. Developmental Psychology, 24(4), 552-559.
[xxi] McNaughton S. (1995). Patterns of emergent literacy. New York: Oxford University Press.
[xxii] Harvey, B. (2002). Managing elevated blood lead levels among young children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta, GA: Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nceh/lead/casemanagement/managingEBLLs.pdf
[xxiii] The Division for Early Childhood of the Council for Exceptional Children. (2016). DEC Recommended Practices with Examples. Retrieved from https://divisionearlychildhood.egnyte.com/dl/NRAghl7roM
[xxiv] The Division of Early Childhood of the Council for Exceptional Children. (2017). Family Capacity-Building Practices Checklist. Retrieved from http://ectacenter.org/~pdfs/decrp/FAM-4_Fam_Capacity-Building_2017.pdf
[xxv] Illinois Department of Human Services Division of Family and Community Services Bureau of Early Intervention (2016). Illinois Early Intervention Provider Handbook. Retrieved from https://blogs.illinois.edu/files/6039/140057/98682.pdf
[xxvi] U.S. Department of Education. (I) Amendments to the Individuals with Disabilities Education Act. IDEA 2004: Building the Legacy Part C (birth – 2 years old). Retrieved from http://idea.ed.gov/part-c/statutes.html
[xxvii] Wisconsin Department of Health Services. (2014). “Developmental Assessment and Intervention for a Child with Lead Exposure.” Wisconsin Childhood Lead Poisoning Prevention Program Handbook. Retrieved from https://www.dhs.wisconsin.gov/publications/p00660-10.pdf
[xxviii] State of Illinois Department of Public Health. (2015). Lead Testing and Case Follow-up Guidelines for Local Health Departments. Retrieved from http://dph.illinois.gov/sites/default/files/publications/lead-testing-and-case-followup-guidelinesfor-local-health-departments-042116.pdf
[xxix] Chicago Department of Public Health (2016). Fifty Years Fighting Lead in Chicago: The Plan for a Lead Free Generation. Retrieved from https://www.cityofchicago.org/content/dam/city/depts/cdph/food_env/general/Lead_Poison_Prevention_Program/CDPH_LeadBrochure_10172016.pdf
[xxx] Elevated Blood Lead Levels are referenced at a confirmed blood lead level greater than or equal to 5 μg/dL of whole blood. (REFERENCE RULE)
[xxxi] Advisory Committee on Childhood Lead Poisoning Prevention of the Centers for Disease Control and Prevention (2012). Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention. Retrieved from https://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf
[xxxii] Centers for Disease Control and Prevention (2016). Water. Retrieved from https://www.cdc.gov/nceh/lead/tips/water.htm
[xxxiii] Zartarian, V. (2017) “Children’s Lead Exposure: A Multimedia Modeling Analysis to Guide Public Health Decision-Making.” Environmental Health Perspectives.
[xxxiv] Commonwealth of Massachusetts Childhood Lead Poisoning Prevention Program. Learn about foods that could keep your child safe from lead poisoning. Retrieved from https://www.mass.gov/service-details/learn-about-foods-that-could-keep-your-child-safe-from-lead-poisoning
[xxxv] Kruse, R. W., & Dubowy, S. M. (2017). Calcium. Kids Health from Nemours. Retrieved from http://kidshealth.org/en/parents/calcium.html
[xxxvi] Gavin, M. L. (2016). Iron. Kids Health from Nemours. Retrieved from http://kidshealth.org/en/parents/iron.html?ref=search
[xxxvii] National Institutes of Health Office of Dietary Supplements (2018). Vitamin C: Fact Sheet for Health Professionals. Retrieved from https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
[xxxviii] University of Illinois Extension. Eat Move Save: Making Healthier Choices on a Budget. Retrieved from https://eat-move-save.extension.illinois.edu/
[xxxix] Nebraska Department of Health & Human Services (2013). Nutrition and Lead Poisoning Prevention. Retrieved from http://dhhs.ne.gov/publichealth/Pages/LeadNutrition.aspx
[xl] Illinois Department of Agriculture. Illinois Products Farmers’ Market LinkUp. Retrieved from https://www2.illinois.gov/sites/agr/Consumers/IllinoisProductsFarmersMarket/Pages/LinkUp.aspx
[xli] Illinois Department of Human Services. Illinois WIC and Senior Farmers’ Market Nutrition Program (FMNP) – DHS 4724. Retrieved from http://www.dhs.state.il.us/page.aspx?item=38054
[xlii] AmpleHarvest.org. Find A Food Pantry Near You. Retrieved from http://ampleharvest.org/find-pantry/
[xliii] Greater Chicago Food Depository. Find Food. Retrieved from https://www.chicagosfoodbank.org/find-food/
[xliv] USDA Food and Nutrition Service. Women, Infants, and Children (WIC). (n.d.). Retrieved from https://www.fns.usda.gov/wic/women-infants-and-children-wic
[xlv] Illinois Department of Human Services. Women, Infants, and Children (WIC). (n.d.). Retrieved from http://www.dhs.state.il.us/page.aspx?item=30513; City of Chicago, Public Health, Healthy Chicago. WIC (Women Infant Children Program. (n.d.). Retrieved from https://www.chicago.gov/city/en/depts/cdph/provdrs/healthymothers_and_babies/svcs/apply_for_wic_.html
The following Illinois Interagency Council on Early Intervention EI and Lead Workgroup Members made significant contributions to the development of these Service Guidelines:
Susan Berger; Associate Professor of Pediatrics and Psychiatry and Behavioral Sciences Northwestern Medicine, Lurie Children’s Hospital
Karen Berman; Director, Illinois Policy Team, Ounce of Prevention Fund
Helen Binns; Professor of Pediatrics and Preventative Medicine Northwestern Medicine, Lurie Children’s Hospital
Bob Cammarata; Program Director, ICG Home Health Care Services
Susan Connor; Director, Early Intervention Training Program, Special Education at the University of Illinois
Benny Delgado; Developmental Therapist and Owner Leaps and Bounds Family Services; President, Developmental Therapy Association
Deanna Durica; Director, Policy Development and Communications at Cook County Department of Public Health
Ann Freiburg; Illinois Department of Human Services, Division of Family and Community Services Bureau Chief of Early Intervention
Meghan Burke; Associate Professor in Special Education, University of Illinois Urbana-Champaign
Samina Hadi-Tabassum; Child Life Specialist Director, Erikson Institute
Nicole Hamp; Developmental-Behavioral Pediatrics Clinical Fellow, University of Michigan C.S. Mott Children’s Hospital
Heather Hofferkamp; Early Intervention Bureau
Maria Kastanis; Assistant Director, Early Intervention Training Program at the University of Illinois
DeeDee Lowery; Manager, Child & Family Connections 1 (CFC 1)
Lori Orr; Preschool Expansion Policy Implementation Director, Office of Early Childhood Development
Stephanie Salgado; Outreach and Education Coordinator, Legal Council for Health Justice
Donna Scherer; Coordinator, Research and Development, Division of Specialized Care for Children
Kristen Schraml; Training Consultant, Early Intervention Training Program at the University of Illinois
Kathy Schrock; Vice President of Clinical Services, Easter Seals DuPage and Fox Valley
Lauren Schroeder; Post-Graduate Teaching Policy Fellow, Civitas Child Law Policy Institute Loyola University Chicago School of Law
Ralph Schubert; Associate Director for Title V Programs, UIC Division of Specialized Care for Children
Nadia Spencer; Provider, Child and Family Connections 5, DuPage County
Kaylan Szafranski; Policy Analyst, Legal Council for Health Justice
Therese Wehman; Professor of Education and Director of MAT and M.Ed. in Early Childhood Education, Elmhurst College
Anita Weinberg; Director at Civitas Child Law Policy Institute Loyola University Chicago School of Law
Amy Zimmerman; formerly of Legal Council for Health Justice
Pamela Epley; Director, Associate Clinical Professor, Director of Special Education, Erikson Institute